- What is Deep Sedation?
Deep sedation is a state of controlled sedation where a patient is in a deep sleep-like state but can be roused with stimulation. It is used to minimize discomfort and anxiety during medical or dental procedures while allowing for rapid recovery.
- How does Deep Sedation work?

Deep sedation works by administering sedative medications that depress the central nervous system. These medications are typically given through intravenous (IV) infusion or inhalation. The goal is to achieve a state where the patient is asleep and relaxed but can be awakened if necessary.
- What are the common medications used in Deep Sedation?
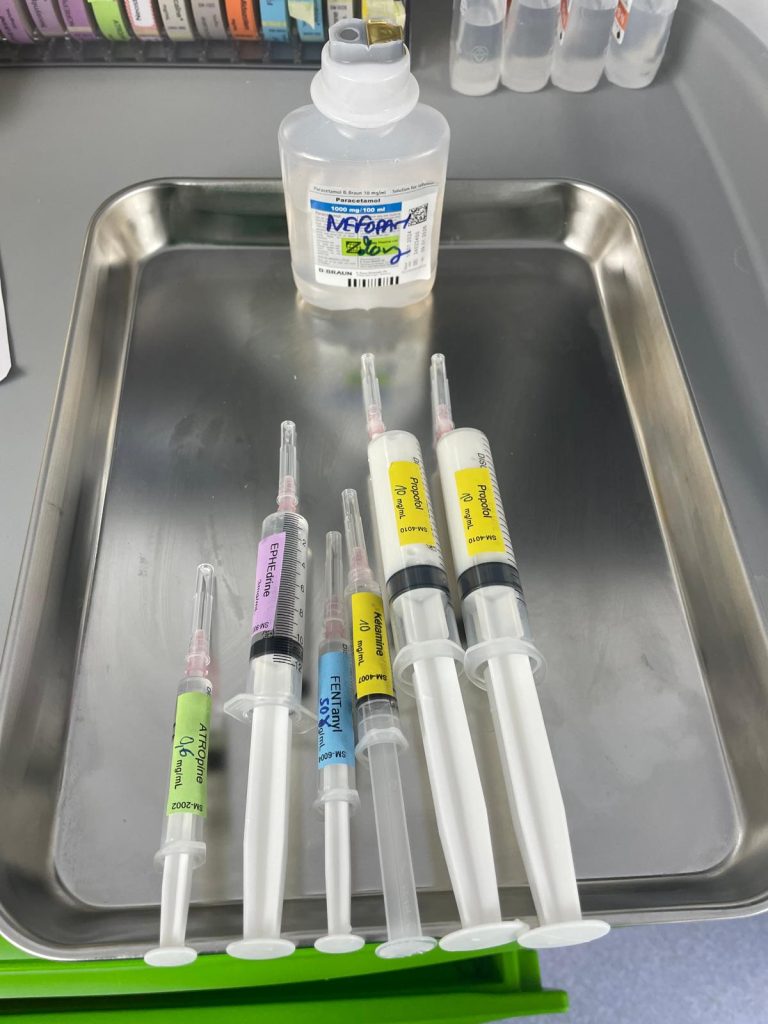
Common medications include:
– Sedatives: Such as propofol, midazolam, or clonidine, which induce a deep sleep-like state.
– Analgesics: Opioids like fentanyl, ketamine or morphine may be used to manage pain during the procedure.
- What are the indications and contraindications?
Deep sedation is a medical state in which a patient is more heavily sedated than in moderate sedation, often resulting in the patient being unaware of their surroundings but still able to respond to stimuli.
Here are some indications and contraindications for deep sedation:
Indications
- Procedures Requiring Patient Stillness: Surgical or diagnostic procedures (e.g., endoscopy, certain dental procedures, short procedure not too painful) that require the patient to remain still.
- Anxiety Management: Patients with severe anxiety or phobia regarding a procedure.
- Pain Management: Procedures that may cause significant discomfort or pain.
- Patient Cooperation Issues: In patients who cannot cooperate due to age (e.g., young children) or mental status.
Contraindications
- Respiratory Compromise: Patients with severe obstructive sleep apnea, chronic obstructive pulmonary disease (COPD), or other significant respiratory issues.
- Cardiovascular Instability: Unstable heart conditions or significant cardiovascular disease.
- Allergies to Sedative Agents: Known allergies or adverse reactions to sedative medications.
- Certain Neurological Conditions: Conditions that could be exacerbated by sedation, such as a history of seizures or altered mental status.
- Pregnancy: Especially in the first trimester, unless absolutely necessary and deemed safe.
- Uncontrolled Diabetes or Thyroid Issues: Conditions that could be exacerbated by sedation.
- Inability to Maintain Airway: In patients who cannot protect their own airway (reflux, obesity BMI>35kg/m2, …), deep sedation can be risky.
Always consult with a qualified healthcare professional to assess the appropriateness of deep sedation for individual patients.
- What can I expect during Deep Sedation?
During the procedure:
– Preparation: You will be monitored continuously. An oxygen mask will be used to administer oxygen.
– Administration: Sedative medications will be administered through an IV line or inhaled, depending on the type of procedure and the age of the patient.
– Monitoring: Your vital signs, including heart rate, blood pressure, and oxygen levels, will be closely monitored throughout the procedure.
– Recovery: After the procedure, you will be monitored as you wake up from the sedation. Recovery times can vary depending on the medications used and the duration of sedation.
- What are the risks and side effects of Deep Sedation?
Risks and side effects may include:
– Respiratory Depression: Slow or difficult breathing, which is managed by monitoring and adjusting sedation levels.
– Low Blood Pressure: A decrease in blood pressure that is monitored and managed by the medical team.
– Nausea and Vomiting: Some patients may experience these symptoms as the sedation wears off.
– Allergic Reactions: Rare but possible reactions to the sedative medications.
– Longer Recovery Time: Depending on the medications used and individual responses.
- How do I prepare for Deep Sedation?
Preparation includes:
– Preoperative Assessment during the preanesthetic consultation: Provide a detailed medical history, including allergies, current medications, last blood tests and any previous reactions to anesthesia or sedation.
– Fasting: Follow instructions on when to stop eating and drinking before the procedure to reduce the risk of complications: typically 6-8 hours prior the surgery (6 hours for light meals, 8h for heavy meals, 2 hours for clear liquids without milk or pulp).
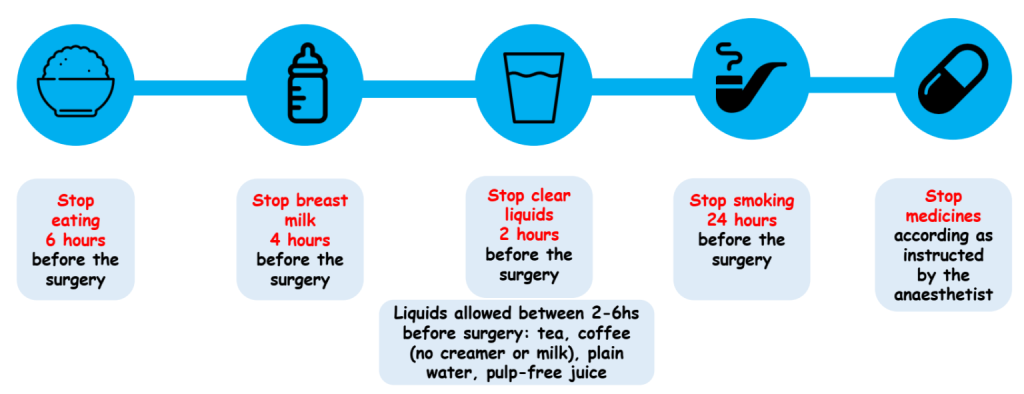
– Medication Review: Inform your healthcare provider about all medications and supplements you are taking.
- What should I do after Deep Sedation?
After deep sedation:
– Recovery: You will need to stay in a recovery area until the effects of the sedation wear off. You may feel groggy or disoriented initially.
– Follow-Up Instructions: Adhere to any specific instructions provided regarding activity levels, diet, and care.
– Arrange Transportation: Since you will not be able to drive, make arrangements for someone to take you home.
- Are there alternatives to Deep Sedation?
Yes, alternatives include:
– Local Anesthesia: Numbs a specific area without affecting consciousness.
– General Anesthesia: Induces a complete loss of consciousness for more extensive procedures.
– Regional Anesthesia: Blocks sensation in a larger area, such as an epidural or spinal anesthesia.
- Can I choose not to have Deep Sedation?
Yes, you can discuss your preferences and concerns with your anesthetist. He will help you understand the best sedation or anesthesia option based on your procedure and medical needs.
- How do I know if deep sedation is safe for me?
Your healthcare provider will evaluate your overall health, medical history, and any risk factors to determine if deep sedation is appropriate and safe for you.
- Where can I get more information?

For more information, consult your anesthesiologist. They can provide detailed explanations tailored to your specific situation and answer any questions you may have regarding deep sedation.
By Dr Solène Paul – Anesthesiologist and Intensive Care physician

Your Health is our mission
