Spinal anesthesia is a regional anesthesia method that provides effective pain relief for surgeries involving the lower body. This approach allows for precise control over pain management while minimizing systemic effects, making it a preferred choice for various procedures, including orthopedic, urological, and gynecological surgeries.
In this section, we will explore the principles of spinal anesthesia, its benefits and risks, the procedure itself, and what patients can expect before, during, and after their surgery. Whether you’re a patient seeking information or a healthcare professional looking to refresh your knowledge, our goal is to equip you with the understanding you need about this important anesthetic technique.
- What is spinal anesthesia?

Spinal anesthesia is a type of regional anesthesia where medication is injected into the cerebrospinal fluid in the spinal canal. The purpose is to block sensation from the waist down. It is often used for surgeries involving the lower abdomen, pelvis, or legs.
- How does Spinal anesthesia work?
Spinal anesthesia involves injecting a local anesthetic into the cerebrospinal fluid in the lower back, specifically into the subarachnoid space. This blocks nerve signals from reaching the brain, providing pain relief and muscle relaxation in the lower part of the body. Depending on the type of local anesthetic used, spinal anesthesia can last from 30 minutes to around 4 hours.
- What are the common medications used in Spinal anesthesia?
Common medications include:
– Local Anesthetics: Such as bupivacaine, or ropivacaine, which numb the area by blocking nerve signals.
– Adjuvants: Medications like fentanyl or clonidine may be added to enhance pain relief and prolong the effects.
- What are the indications and contra-indications please?
– Indications:
* Spinal anesthetics can often be used in isolation as the sole anesthetic or with sedation for patient comfort.
* Typical surgical indications for spinal anesthesia include lower abdominal, perineal, and lower extremity surgery.
* Epidural anesthetics are often used as an adjunct to spinal or systemic anesthesia and can include thoracic, abdominal, or lower extremity surgery. This can be performed with a single procedure known as a CSE (combined spinal-epidural).
– Contraindications:
Absolute contraindications
* Patient refusal
* Allergy to medication used
* Infection at the site
* Severe coagulation abnormalities
* Critical/severe aortic stenosis and high intracranial pressure
* Spinal Metastases near the level of approach
Relative contraindications
* Spinal abnormalities
* Previous spine surgery at the desired target
* Coagulopathy
* Fixed cardiac output states
* Active infections.
* Autoimmune neurologic disorders may pose an undue risk, and careful consideration of risks and benefits must be weighed.
- What can I expect during the procedure?
During the procedure:
– Preparation: You will be positioned, often sitting up or lying on your side. To facilitate the puncture, you must round your back to open the vertebrae and allow the needle to be inserted.

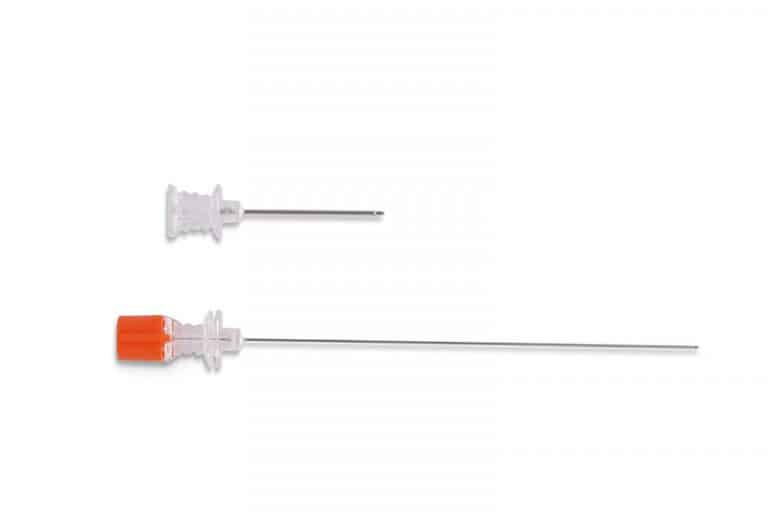
– Injection: The anesthesiologist will disinfect the area on your lower back and insert a needle into the spinal canal to administer the anesthetic.
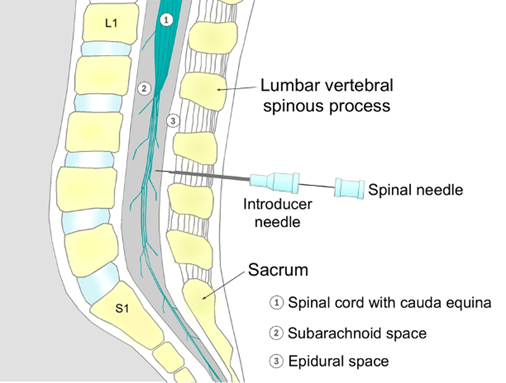
– Onset: You will begin to feel numbness and loss of sensation in the lower body within 5 minutes.
- What are the risks and side effects of spinal anesthesia?
Risks and side effects may include:
– Headache: A post-dural puncture headache (PDPH) may occur if there is a leak of cerebrospinal fluid.
– Back Pain: Mild soreness at the injection site.
– Nausea: Some patients may feel nauseated.
– Low Blood Pressure: The anesthetic can cause a drop in blood pressure.
– Rare Complications: Including infection, bleeding, or nerve damage.
- How do I prepare for spinal anesthesia?
Preparation includes:
– Preoperative assessment during the preanesthetic consultation: Discuss your medical history, current medications, last blood test results and allergies with your anesthesiologist.
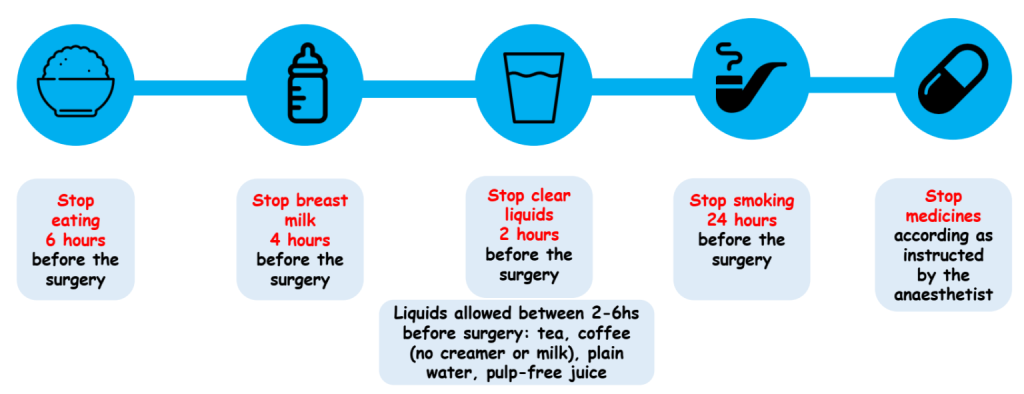
– Fasting: Follow instructions on when to stop eating and drinking before the procedure: typically 6-8 hours prior the surgery (6 hours for light meals, 8h for heavy meals, 2 hours for clear liquids without milk or pulp).
– Medication Review: Inform your healthcare provider about any medications or supplements you are taking.
- What should I do after the procedure?
After the procedure:
– Recovery Time: You will need to lie flat to allow the anesthetic to take full effect.
– Observation: You will be monitored for any immediate side effects or complications.
– Follow-Up Instructions: Adhere to any specific instructions regarding movement, activity, and pain management.
- Are there alternatives to spinal anesthesia?
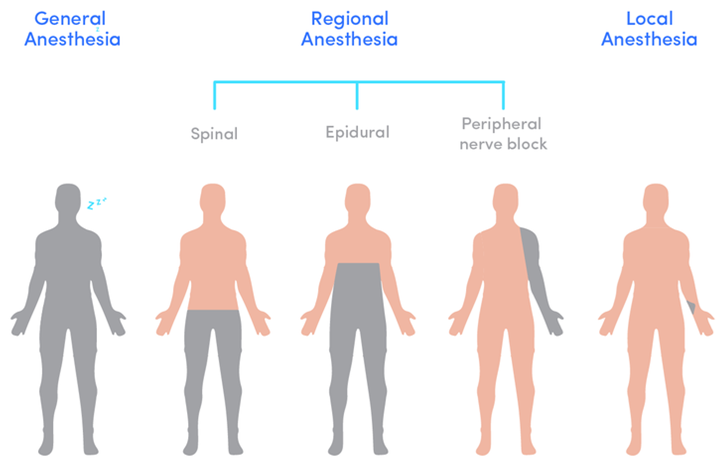
Yes, alternatives include:
– Epidural Anesthesia: Similar to spinal anesthesia but the medication is injected into the epidural space rather than the subarachnoid space.
– General Anesthesia: Induces a state of unconsciousness and is used for a wider range of surgeries.
– Local Anesthesia: Numbs a small area of the body, but you remain awake and aware.
– Regional Anesthesia: Blocks sensation in a larger area.
- Can I choose not to have spinal anesthesia?
Yes, you can discuss your preferences and concerns with your anesthetist. He will help you understand the best anesthesia option for your procedure based on its type, duration, and your overall health.
- How do I know if spinal anesthesia is safe for me?
Your anesthesiologist will assess your health history, current medical conditions, and any risk factors to determine if spinal anesthesia is appropriate and safe for you.
- Where can I get more information?
For more information, consult your anesthesiologist. They can provide detailed explanations and answer any specific questions you may have regarding spinal anesthesia.
By Dr Solène Paul – Anesthesiologist and Intensive Care physician

Your health is our mission
