- What is Epidural Anesthesia?
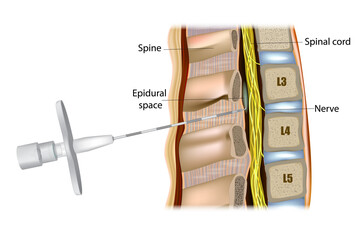
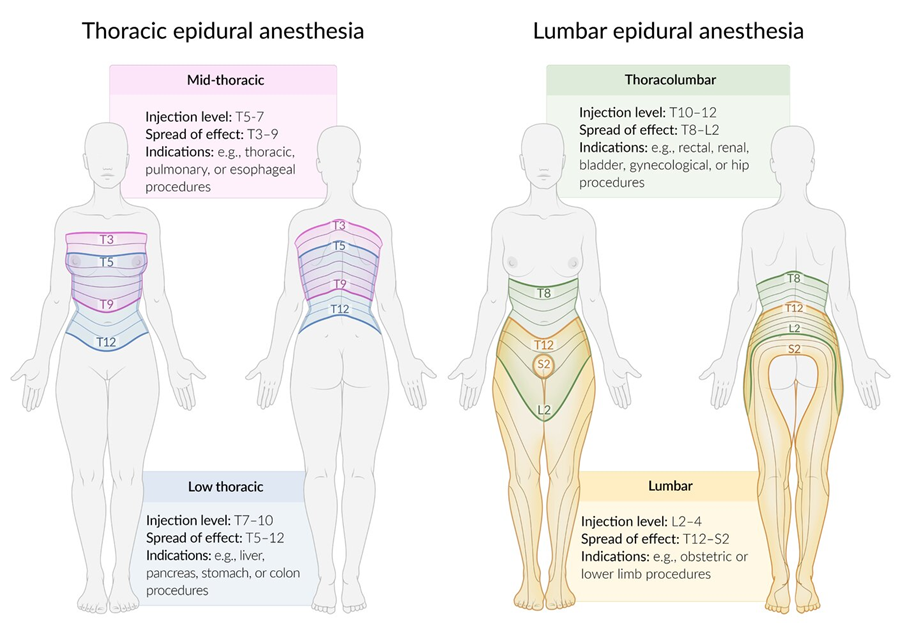
Epidural anesthesia is a form of regional anesthesia that involves injecting an anesthetic drug into the epidural space around the spinal cord. This technique blocks sensation in the lower part of the body, often used for pain relief during labor and delivery or certain types of surgery.
- How does Epidural Anesthesia Work?
Epidural anesthesia works by delivering anesthetic medication into the epidural space. This blocks nerve signals from reaching the brain, leading to numbness and pain relief in the lower body. The patient remains conscious but does not feel pain in the targeted area.
- What are the indications and contraindications?
Epidural anesthesia is commonly used for pain relief during labor and certain surgical procedures. Here are the indications and contraindications:
Indications
- Labor Pain Relief: To provide analgesia during childbirth.
- Surgical Procedures: Used for lower abdominal, pelvic, or lower limb surgeries.
- Chronic Pain Management: For conditions like chronic back pain.
- Postoperative Pain Control: Helps manage pain after surgery, particularly in the lower body.
- Certain Medical Conditions: Can be beneficial in patients with specific medical conditions requiring regional anesthesia.
Contraindications
- Severe Spinal Deformities: May complicate access to the epidural space.
- Coagulation Disorders: Conditions that affect blood clotting, increasing the risk of hematoma.
- Infection at the Injection Site: Increased risk of infection in the epidural space.
- Allergy to Anesthetics: Hypersensitivity to local anesthetics used in the procedure.
- Severe Hypotension: Conditions leading to critically low blood pressure.
- Neurological Disorders: Certain neurological issues can increase risk.
- Patient Refusal: If the patient does not consent to the procedure.
- What are the common medications used in Epidural Anesthesia?

Common medications include:
– Local Anesthetics: Such as lidocaine, bupivacaine, or ropivacaine, which block nerve signals.
– Analgesics: Opioids like fentanyl or morphine may be added to enhance pain relief and reduce the amount of local anesthetic needed.
- What can I expect during the procedure?

During the procedure:
– Preparation: You will be positioned, often sitting or lying on your side, to access the epidural space in the lower back. It is necessary to bend the back in order to open the vertebrae to allow better insertion of the needle.

– Injection: The anesthesiologist will clean the area, insert a needle into the epidural space after a local anesthesia of your skin, and then thread a thin catheter through the needle to administer the anesthetic drug. The procedure is painless.
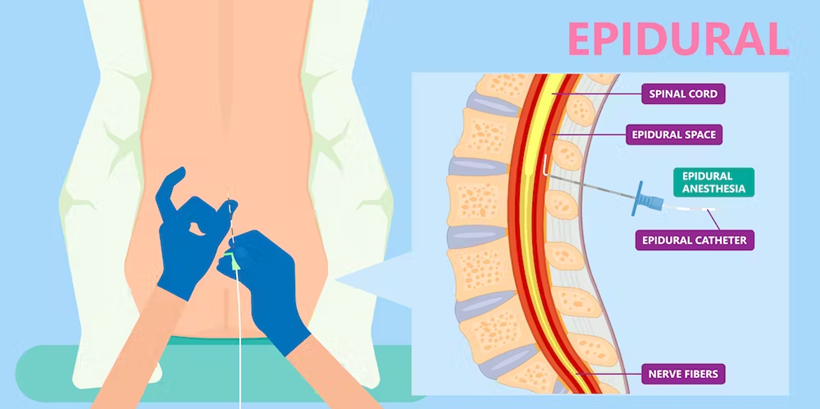
– Onset: You will begin to feel numbness and loss of sensation in the lower part of your body within 10-20 minutes.
– Epidural pump PCEA (Patient Controlled Epidural Analgesia): The local anesthetic is injected into the catheter located in the epidural space using a syringe pump that delivers a continuous flow. If necessary, the patient can add boli by pressing a button. There is no risk of overdose because the dose limits that must not be exceeded are entered into the syringe pump.
- What are the risks and side effects of Epidural Anesthesia?
Risks and side effects may include:
– Back Pain: Mild soreness at the injection site sometimes.
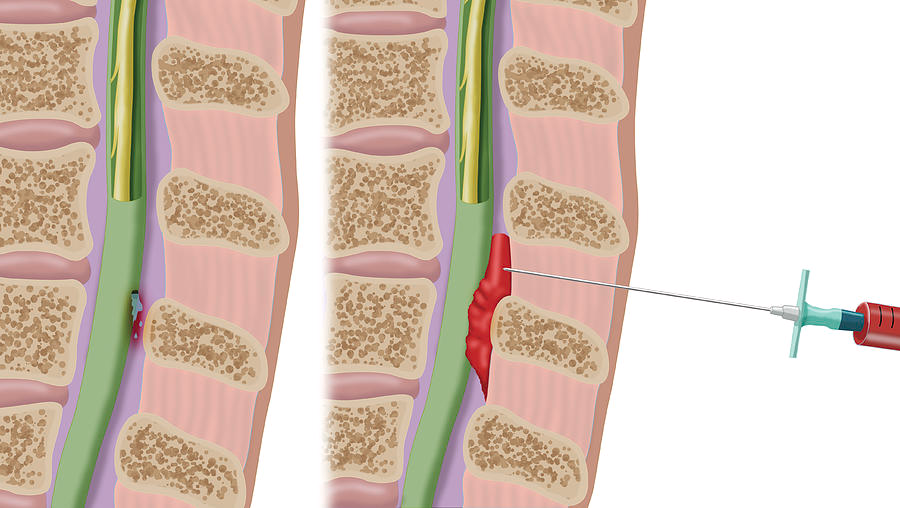
– Headache: A post-dural puncture headache (PDPH) if the needle accidentally punctures the dura mater (less common).
The dura mater breach consists in going too far with the epidural needle into the spinal canal, as in spinal anesthesia. The epidural needle is larger than the spinal needle. This creates a small hole in the dura mater which, when raised, causes the brain to be pulled downwards by the pressure difference, resulting in headaches. This small hole can be closed by injecting blood into the back (blood patch) if the headaches are too severe. If nothing is done, it will close up by itself within a few days.
– Low Blood Pressure: The anesthetic can cause a drop in blood pressure.
– Nausea or Vomiting: Some patients may experience these symptoms.
– Rare Complications: Including infection, bleeding, or nerve damage.
- How do I prepare for Epidural Anesthesia?
Preparation includes:
– Anesthesia consultation 3-4 weeks before the estimated date of delivery (EDD): Discuss your medical history, current medications, last blood test results and allergies with your anesthesiologist.
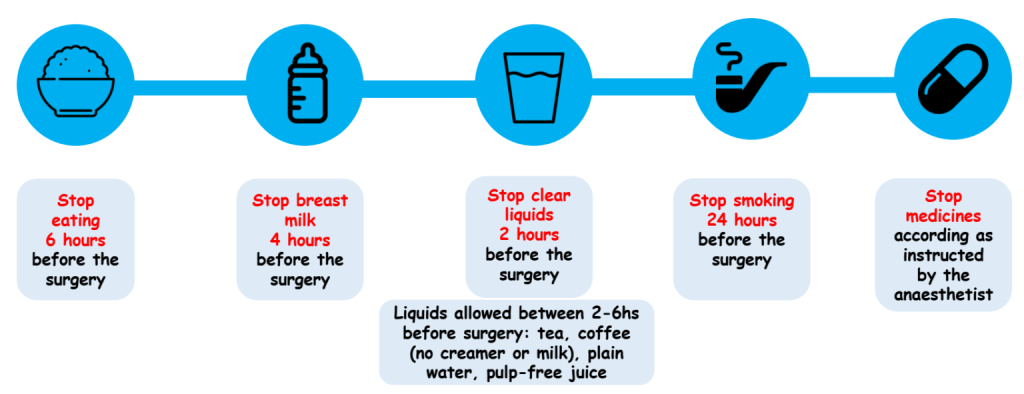
– Fasting: Follow instructions on when to stop eating and drinking before the procedure: typically 6-8 hours prior the surgery (6 hours for light meals, 8h for heavy meals, 2 hours for clear liquids without milk or pulp).
– Medication Review: Inform your healthcare provider about any medications or supplements you are taking. Your anesthesiologist will tell you what medication to stop before your surgery to ensure your safety.
- When can I request an Epidural?

The epidural is administered by an anesthetist during labor, generally between 3 and 8 cm of dilation.
We don’t place the epidural before 3 cm to make sure you’re not in false labor.
After 8 cm, the epidural may not have enough time to be effective for delivery. However, it is possible to use spinal anesthesia with a small dose of local anesthetic to avoid pain but still be able to push for delivery.
For surgery, epidurals are done under local anaesthesia prior to general anaesthesia.
- How long can I keep the Epidural catheter?
During obstetrical labor, you’ll keep it on for up to two hours after delivery.
After surgery, the catheter can be removed 24 to 72 hours after surgery, depending on pain. There is no maximum duration for keeping an epidural catheter. Nevertheless, as a precautionary measure, it should be kept in place only as long as necessary.
- Are there alternatives to Epidural anesthesia?
Yes, epidurals are not compulsory so there are some alternatives.
LABOUR
Yes, there are several alternatives to epidurals for pain management during childbirth. Here are just a few:
– Intravenous analgesia: Medications such as pethidine can be administered intravenously to relieve pain.
– Laughing gas (nitrous oxide): Used to reduce anxiety and pain, it is inhaled by the patient.
– Relaxation techniques: Methods such as deep breathing, meditation or hypnosis can help manage pain.
– Acupuncture and acupressure: These traditional methods can be effective in relieving pain.
– Massage: Massage by a partner or professional can bring some relief.
– Hot bath or shower: Warm water can help relax muscles and reduce pain.
– Positioning: Changing position or using a birth ball can contribute to greater comfort.
It’s important to discuss these options with your healthcare professional to find the best solution for you.
SURGERY
There are several alternatives to epidurals for pain management after surgery, including:
- Oral Medications
- Intravenous (IV) Medications
- Patient-Controlled Analgesia (PCA): This allows patients to self-administer a preset dose of pain medication via an IV pump.
- Regional Anesthesia: Techniques such as femoral nerve blocks or brachial plexus blocks can be used depending on the surgery location.
- Physical Therapy: Early mobilization and guided exercises can aid recovery and pain management.
- Complementary Therapies: Methods like acupuncture, mindfulness, and relaxation techniques may also provide relief.
It’s essential to discuss pain management options with your healthcare provider to find the best approach for your specific situation.
- Does Epidural anesthesia slow obstetrical labour and increase the risk of cesarean section?
Epidural anesthesia does not increase the risk of cesarean section. It may slightly slow obstetrical labor.
- Can I choose not to have Epidural anesthesia?
Yes, epidurals are not mandatory. There are there to relieve you. You can discuss your preferences and concerns with your anesthetist. He will help you understand the best anesthesia option based on your procedure and health status.
- What is the difference between Spinal and Epidural anesthesia?
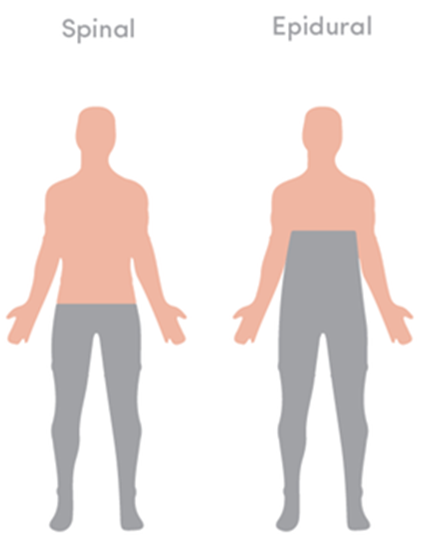
Indications are different between an Epidural and a Spinal anesthesia:
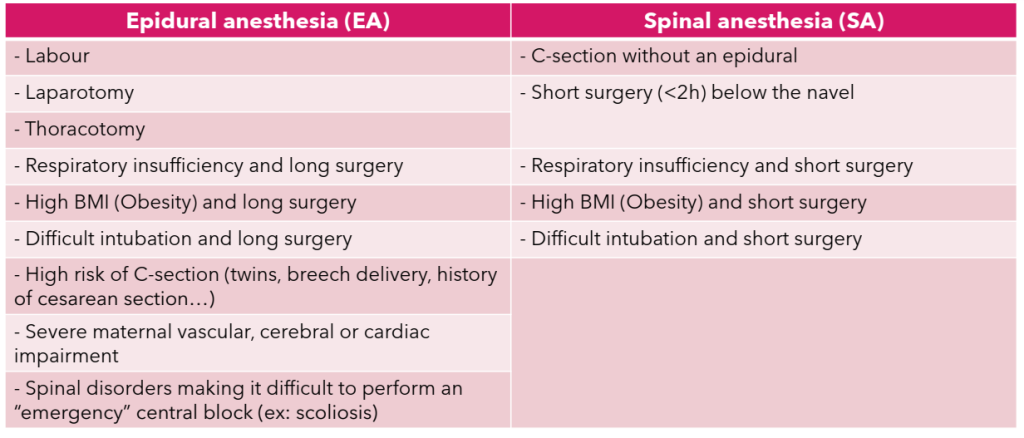
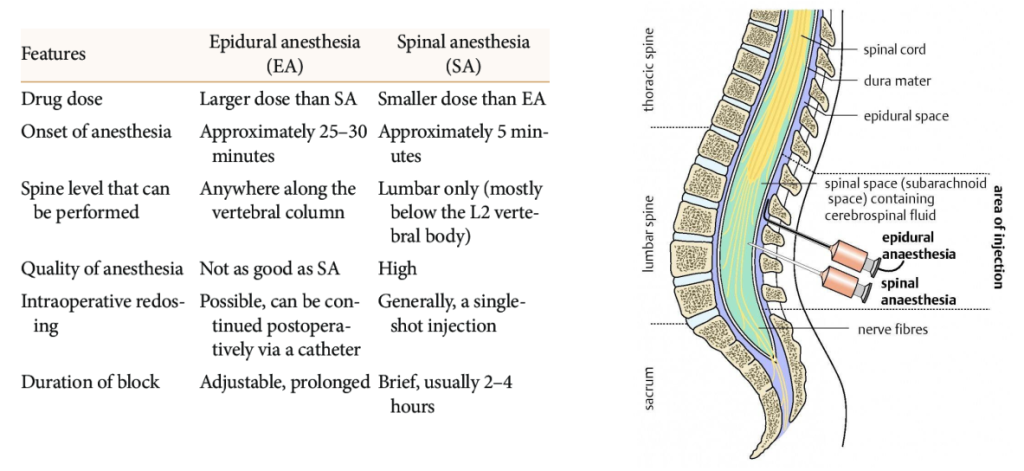
The depth of puncture is not the same. The spinal needle is deeper. It goes all the way into the spinal canal, where the cerebrospinal fluid is located.
Spinal anesthesia therefore has a shorter, more effective action time.
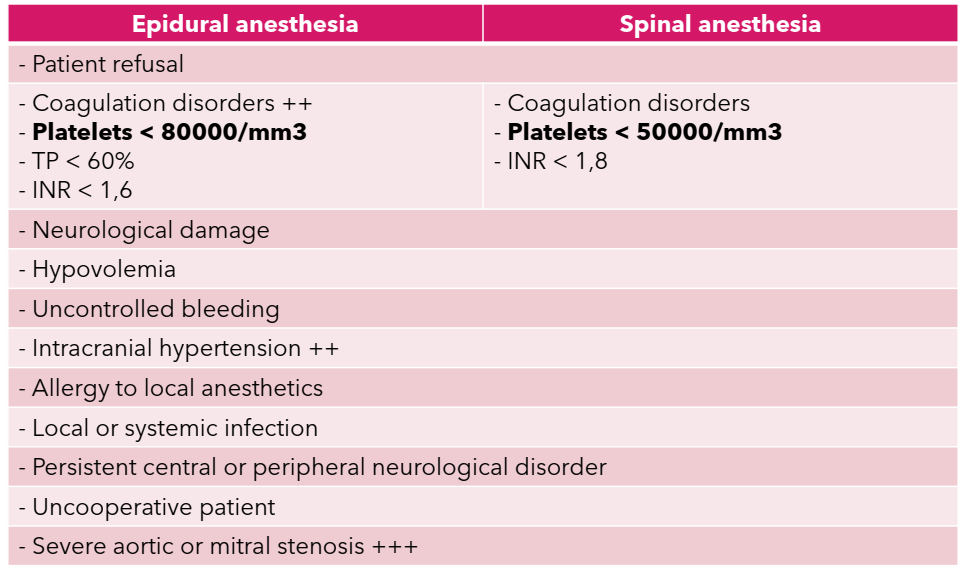
The contraindications are almost the same.
- How do I Know if Epidural Anesthesia is safe for me?
Your anesthesiologist will evaluate your health history, current medical conditions, last blood test and any risk factors to determine if epidural anesthesia is appropriate and safe for you.
- Where can I get more information?
For more information, consult your anesthesiologist. They can provide detailed explanations tailored to your specific situation and answer any questions you may have regarding epidural anesthesia.
By Dr Solène Paul – Anesthesiologist and Intensive Care physician

Your health our mission
