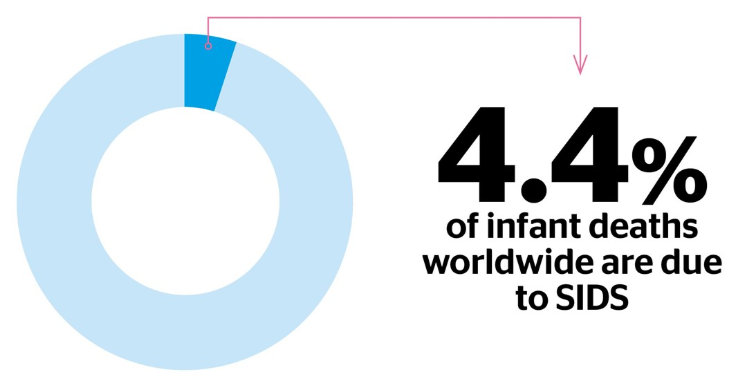
Becoming a parent is one of life’s most rewarding experiences — but it also comes with questions, worries, and responsibilities. One topic that often causes concern for new and expectant parents is Sudden Infant Death Syndrome (SIDS).
In this article, we’ll explore what SIDS is, what we know about it, and — most importantly — what you can do to help reduce your baby’s risk.
1. What is SIDS?
Sudden Infant Death Syndrome, sometimes referred to as “cot death”, is the sudden and unexplained death of a healthy baby, usually during sleep, and typically in babies under one year of age. Most cases occur between the ages of 2 and 4 months, and it’s slightly more common in boys than in girls.

While the exact cause of SIDS is still unknown, research suggests that it likely results from a combination of factors, including:
- A baby’s vulnerability during a critical stage of development
- Environmental stressors, such as sleeping position or overheating
- Possible underlying health conditions or immature cardiorespiratory systems

2. How to Reduce the Risk of SIDS
Fortunately, there are several evidence-based steps parents and caregivers can take to create a safer sleep environment and help reduce the risk of SIDS.
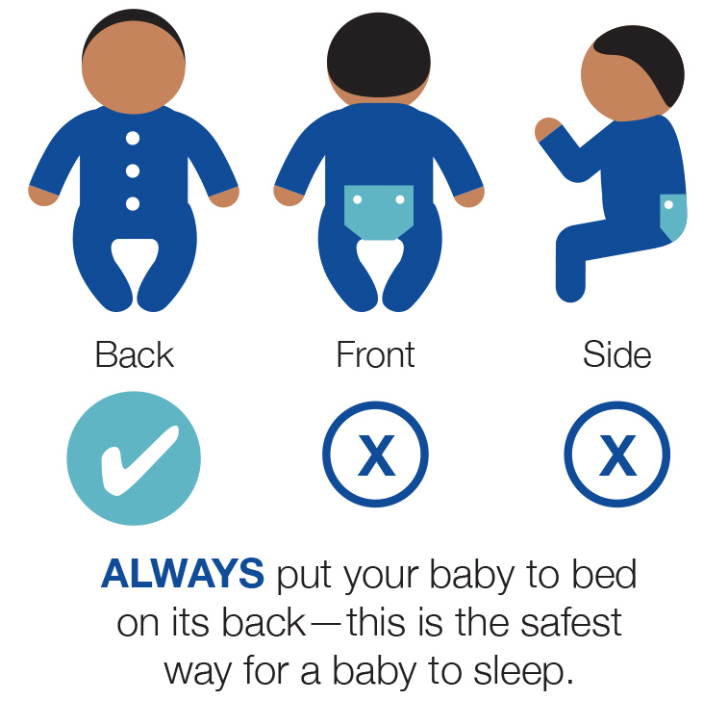
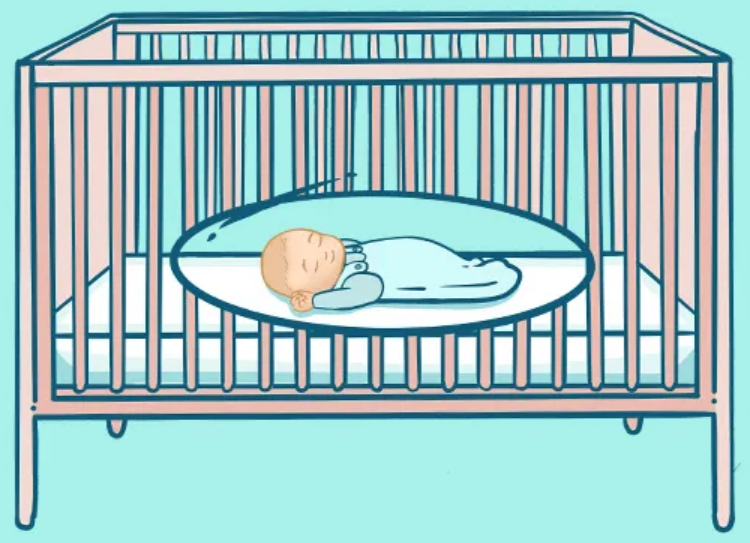
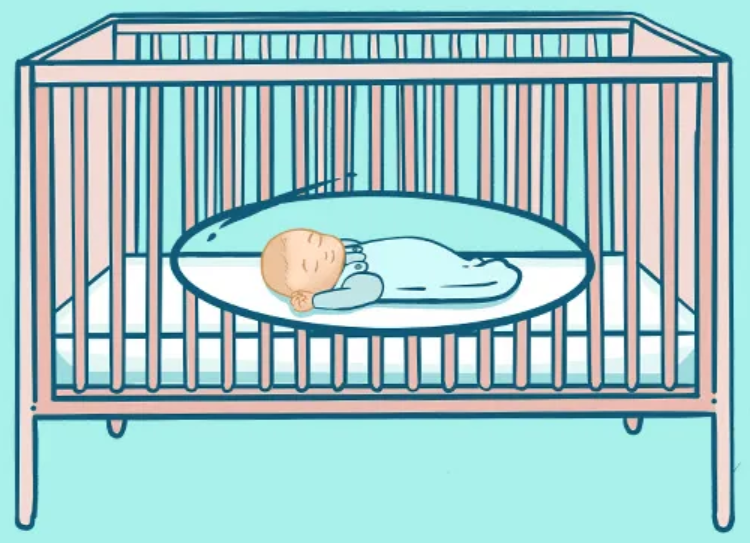
1. Always place your baby on their back to sleep
This is the number one recommendation from pediatric associations worldwide. Placing your baby on their back (not on their side or tummy) reduces the risk of suffocation or rebreathing carbon dioxide.

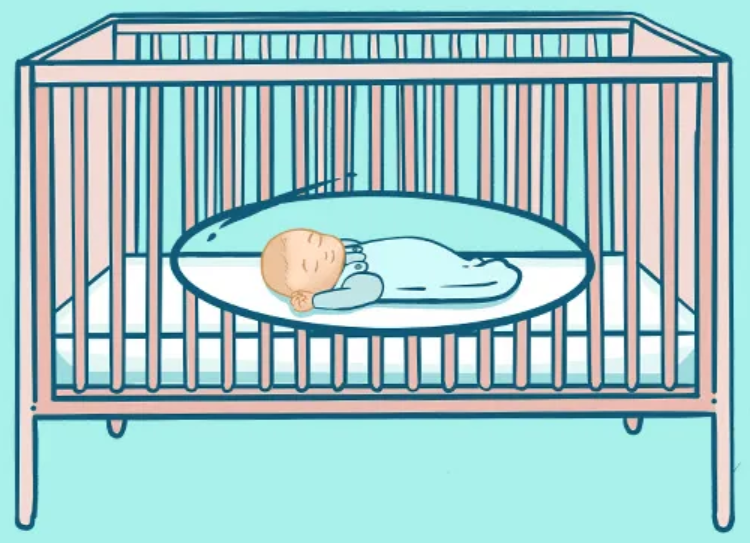
2. Use a firm, flat sleep surface
Place your baby in a crib, bassinet, or cot with a firm mattress and a fitted sheet. Avoid soft bedding, pillows, stuffed toys, and crib bumpers, which can pose suffocation hazards.
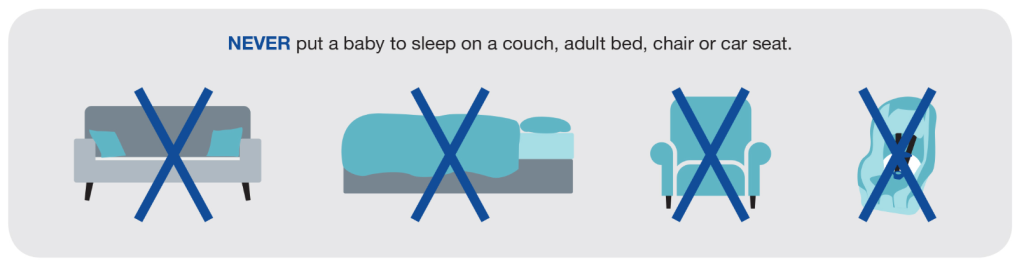
Using a car seat for travel is important for infant safety, but prolonged or unsupervised sleep in a car seat can increase the risk of SIDS and positional asphyxia. Experts recommend transferring a sleeping baby to a firm, flat sleep surface as soon as possible after travel.
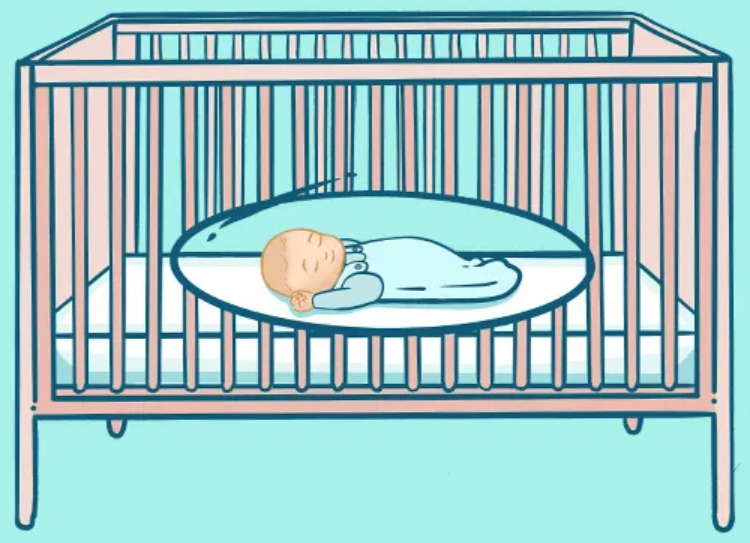
3. Keep the crib clear and simple
The safest crib contains:
- Baby in a sleep sack or wearable blanket
- No loose blankets, toys, or pillows
- A flat surface, free from inclines

Don’t use a loose blanket but a wearable blanket or a sleeping bag.

4. Share a room, not a bed
The AAP recommends that babies sleep in the same room as their parents (but not in the same bed) for at least the first 6 months, and ideally for the first year.

5. Avoid overheating
Dress your baby appropriately for the room temperature. Signs of overheating include sweating, flushed cheeks, and rapid breathing. Keep the room at a comfortable temperature (typically 18–20°C or 65–68°F).
6. Breastfeeding lowers risk
Exclusive breastfeeding for the first 6 months has been associated with a significantly lower risk of SIDS. Even partial breastfeeding provides protective benefits.

7. Offer a pacifier at sleep time
Using a clean, dry pacifier at nap and bedtime may reduce the risk of SIDS, even if it falls out after the baby is asleep. If you are breastfeeding, wait until breastfeeding is well established (usually around 3–4 weeks) before introducing a pacifier.

8. Avoid smoking and exposure to smoke
Babies who are exposed to cigarette smoke—before or after birth—are at much higher risk of SIDS. Keep your baby’s environment smoke-free.

8. Tummy time
Tummy time helps prevent SIDS (Sudden Infant Death Syndrome) by strengthening a baby’s neck, shoulder, and core muscles, which promotes healthy motor development and reduces the risk of suffocation during sleep. While babies should always sleep on their backs, supervised tummy time while awake is essential for their safety and development.
Tummy time decreases the risk to have a plagiocephaly or brachycephaly.
3. Myths and Misconceptions
There are many myths around SIDS. Let’s clarify a few:
- “It only happens at night.” False. SIDS can happen during daytime naps too.
- “It runs in families.” While there may be genetic vulnerabilities, SIDS is not hereditary in the traditional sense.
- “Using monitors can prevent SIDS.” Home apnea monitors have not been proven to reduce the risk of SIDS.
4. Final Thoughts
SIDS is rare — and it’s getting rarer. Thanks to decades of research and public health campaigns like “Back to Sleep,” the rates of SIDS have dropped dramatically.
Still, it’s important to stay informed and proactive. By following the latest safety guidelines and creating a safe sleep environment, you can rest easier knowing you’re doing everything possible to protect your baby.

5. Resources and Support
If you’re a new parent and feel overwhelmed, you’re not alone. Speak with your pediatrician or healthcare provider if you have concerns.
Here are a few helpful resources: