Pain can take many forms — aching, burning, stabbing — but one thing is certain: when it interferes with your daily life, it needs to be addressed. Whether acute or chronic, nociceptive or neuropathic, effective pain management relies on understanding what type of pain you’re dealing with and choosing the right treatment strategy.
1. What is Pain?
Pain is the body’s alarm system, signaling that something might be wrong. It can arise from tissue damage (nociceptive pain), nerve injury (neuropathic pain), or a combination of both.
2. Types of Pain
🔹 Nociceptive Pain
- Caused by tissue injury or inflammation
- Feels sharp, aching, or throbbing
- Examples: post-surgical pain, arthritis, injuries
🔹 Neuropathic Pain
- Caused by nerve damage or dysfunction
- Feels burning, shooting, electric-like
- Examples: diabetic neuropathy, sciatica, shingles
3. The Pain Scale (0–10)
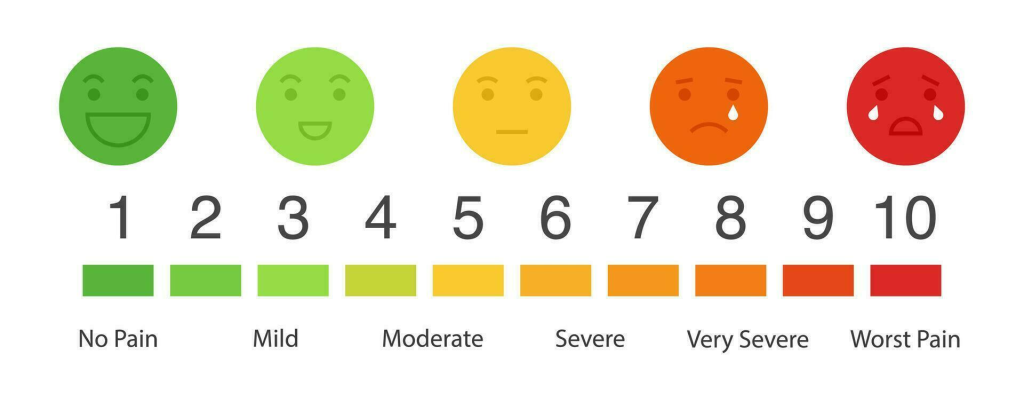
| Level | Description | Impact on Life |
|---|---|---|
| 0 | No pain | — |
| 1–3 | Mild pain | Manageable, may be annoying |
| 4–6 | Moderate pain | Disrupts activities and focus |
| 7–10 | Severe pain | Debilitating, may require urgent care |
Healthcare professionals use this scale to adjust pain treatment to your needs.
4. Painkillers by Pain Level
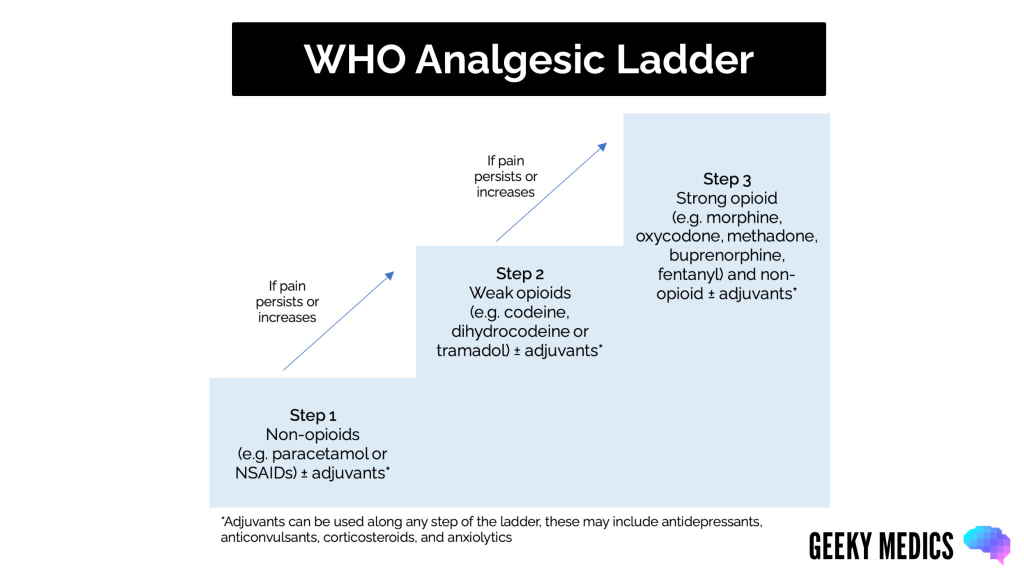
This step-by-step approach is designed to match the intensity of the pain with the appropriate level of medication:
🟢 Step 1: Mild Pain (Score 1–3)
- Non-opioid analgesics
- Paracetamol (acetaminophen)
- NSAIDs (e.g., ibuprofen, naproxen)
- Nefopam (acupan)
- Often enough for minor injuries, headaches, or mild arthritis
🟡 Step 2: Moderate Pain (Score 4–6)
- Weak opioids + non-opioids
- Codeine, tramadol (with or without paracetamol)
- Continue with NSAIDs or paracetamol for synergy
- Suitable for moderate post-surgical pain, fractures, dental procedures
🔴 Step 3: Severe Pain (Score 7–10)
- Strong opioids
- Morphine, oxycodone, hydromorphone, fentanyl
- Typically used for cancer pain, post-operative pain, or trauma
- Often combined with Step 1 medications for enhanced relief
- Requires close monitoring for side effects like sedation, nausea, and respiratory depression
⚠️ Note: Opioids are powerful tools, but they must be used cautiously due to the risk of tolerance, dependence, and overdose. A doctor will determine the correct dose and duration.
5. Neuropathic Pain Requires Special Treatment
Neuropathic pain does not always respond well to typical painkillers. Instead, doctors often prescribe:
- Antidepressants: e.g., amitriptyline, duloxetine
- Anticonvulsants: e.g., gabapentin, pregabalin
- Topical agents: lidocaine patches, capsaicin cream
These work by calming overactive nerves rather than numbing pain.
6. Non-Medication Strategies
A well-rounded pain management plan often includes:
- Physical therapy
- Heat or cold therapy
- Acupuncture or massage
- Interventional techniques: like nerve blocks or epidural injections
7. When to Seek Help
- Pain persists more than a few weeks
- It’s affecting sleep, mobility, or mental health
- You experience numbness, tingling, or unexplained weakness
A healthcare professional can help tailor a plan using a combination of medications, therapies, and lifestyle changes.
8. Final Takeaways
- Pain is complex — and so is its treatment.
- The pain scale helps guide safe and effective care.
- Different types of pain (nociceptive vs. neuropathic) require different approaches.
- The goal is always to improve comfort, function, and quality of life.
You don’t have to suffer in silence. Pain is treatable — and with the right support, relief is within reach.
